Meeting Date: May 1, 2019
Report No. BH.01.MAY0119.R13
Prepared By: Dr. Matthew Tenenbaum, Associate Medical Officer of Health and Karen Mulvey, Interim Clinical Services Manager
Approved By: Rita Isley, Director of Community Health and Chief Nursing Officer
Submitted By & Signature: Dr. Nicola J. Mercer, MD, MBA, MPH, FRCPC Medical Officer of Health & CEO
Recommendations
It is recommended that the Board of Health:
- Receive this report for information.
Key Points
- Chlamydia and gonorrhea infections are increasing in Wellington, Dufferin and Guelph (WDG), though local rates are lower than provincial rates. These infections are generally seen in younger age groups. Multiple reasons account for increasing infection rates across the country.
- Infectious syphilis is much less common in WDG and the small number of cases makes it difficult to draw conclusions about trends over time. The tendency for cases to be older and male reflects the trend in North America, over the past few years of infectious syphilis emerging among men who have sex with men (MSM).1
- Trends in sexual risk behaviours are changing. Survey data found a significant increase in the proportion of people who reported not using condoms, which may contribute to trends in STIs.
- STI surveillance helps to inform program delivery. This data informs the sexual health services delivered by the Clinical Services team.
Discussion
Chlamydia
Chlamydia is a bacterial infection spread through vaginal, anal or oral sex.2 Most individuals with chlamydia have no symptoms, though the infection can cause pain during urination and discharge from the penis or vagina. Complications include pelvic infections, which can cause infertility or chronic pelvic pain.3 Chlamydia can be tested with urine specimens, cervical swabs, rectal swabs, and/or throat swabs. Positive test results are reported to Wellington-Dufferin-Guelph Public Health (WDGPH). Safer sex practices (such as condom use) reduce the risk of transmission. Chlamydia infections can be treated with antibiotics, though a person who has been treated may be re-infected if they are exposed again.3
Key findings from local data reveal that:
- Rates of chlamydia are increasing in WDG, consistent with national and provincial trends;
- Rates in WDG are lower than provincial rates;
- Rates were highest in younger age groups; and
- Females accounted for more reported cases than males.
Trends Over Time (2008-2018):
Over the past decade, rates of chlamydia infections have increased in Ontario and Canada.4 A similar trend has been observed in WDG since 2008. The unadjusted rate increased 97% from 139 cases per 100,000 people in 2008 to 273 cases per 100,000 people in 2018. The rate in WDG was consistently lower than the provincial rate during this time (Figure 1). Adjustments to account for age differences between the WDG and Ontario populations do not significantly change these rates.
Figure 1: Crude rates of Chlamydial infection, Wellington-Dufferin-Guelph and Ontario, 2008-2018
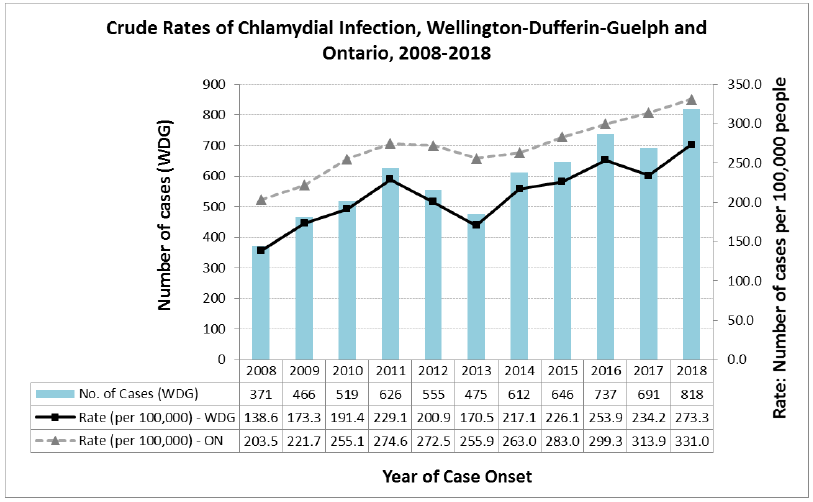
Changes in chlamydia rates over time have been well-studied and increasing rates are likely due to a combination of factors including:
- Changes in sexual behaviours (such as condom use) that modify the risk of transmission;
- Greater rates of re-infection after treatment, as cases return to their sexual networks;
- More accurate, available and acceptable testing methods that allow more infections to be counted as cases; and
- More effective screening and contact tracing practices.4
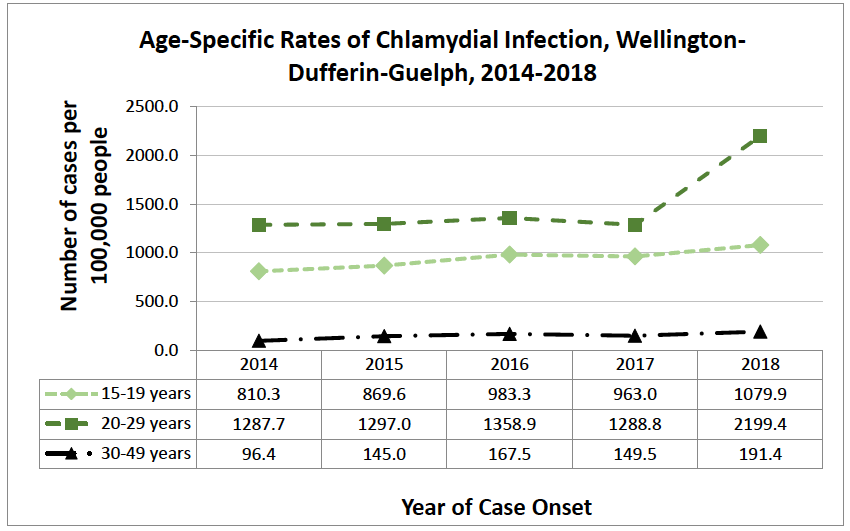
Rates by Age (2014-2018):
Sexually active youth and young adults are most likely to be infected with chlamydia. In WDG, the rate of infection is highest in the 20-29-year-old age group, followed by the 15-19-year-old age group. Infection rates are much lower in the 30-49-year-old age groups and in other age groups (Figure 2).
In 2018, there was a sharp increase in the rate of reported chlamydial infections in the 20-29-year-old age group. The cause of this increase is uncertain, but it may be due to enhanced testing services offered through outreach programs, at community events, and to the university population in the City of Guelph.
Figure 2: Age-Specific Rates of Chlamydial Infection, Wellington-Dufferin-Guelph, 2014-2018.
Rates by Gender (2014-2018):
The distribution of chlamydia infections between males and females has been consistent across the past five (5) years (2014-2018), with approximately 60% of cases in females and 40% in males each year. This is consistent with national and provincial findings and likely reflects the fact that females are more likely than males to be screened for STIs.4
Gonorrhea
Gonorrhea is a bacterial infection which, like chlamydia, is spread through vaginal, anal or oral sex.5 Infected females are often asymptomatic, though infected males often experience painful urination or discharge from the penis. Like chlamydia, gonorrhea can progress to pelvic infection or cause infertility.6 Gonorrhea testing is often done alongside chlamydia testing using urine specimens, cervical swabs, rectal swabs, and/or throat swabs. Positive test results are reported to WDGPH. Safer sex practices (such as condom use) reduce the risk of transmission. Gonorrhea infections can be treated with antibiotics, though rates of resistance are increasing in Canada.6
Key findings from local data reveal that:
- Rates of gonorrhea are increasing in WDG, consistent with national and provincial trends;
- Rates in WDG are lower than provincial rates;
- Rates were highest in younger age groups; and
- Males accounted for more reported cases than females.
Rates Over Time (2008-2018):
Rates of gonorrhea infection are much lower than rates for chlamydia. Like chlamydia, however, rates have been increasing in WDG in keeping with trends seen across the country.4 The unadjusted rate increased 204% from 11 cases per 100,000 people in 2008 to 34 cases per 100,000 people in 2018. The rate in WDG was consistently lower than the provincial rate during this time (Figure 3). Adjustments to account for age differences between the WDG and Ontario populations do not significantly change these rates.
Figure 3: Crude Rates of Gonorrhea Infections, Wellington-Dufferin-Guelph and Ontario, 2008-2018.
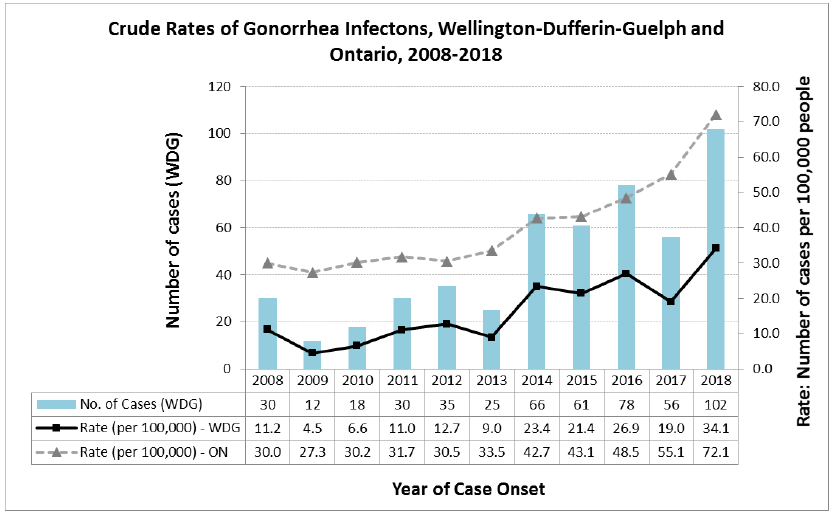
Factors driving increased gonorrhea rates are generally thought to be similar to the same factors causing increased chlamydia rates.4
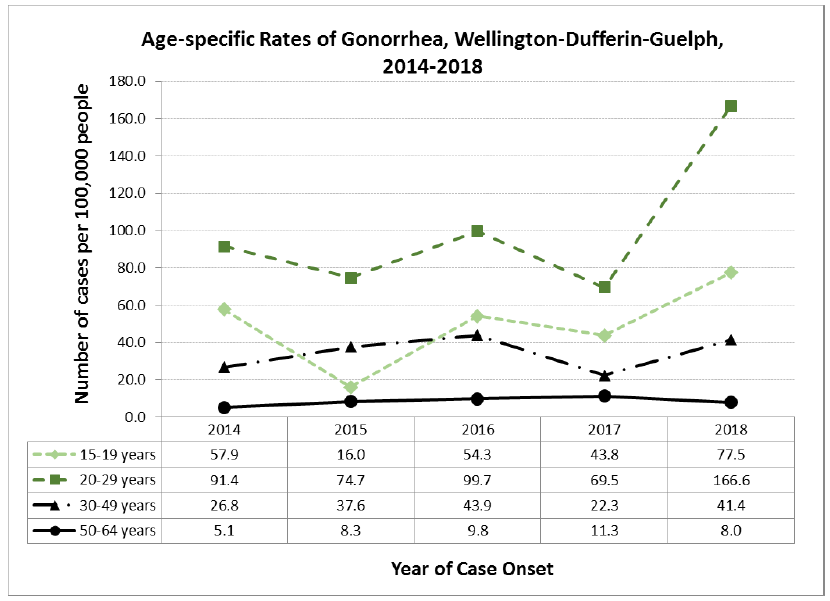
Rates by Age (2014-2018):
Trends by age for gonorrhea are quite similar to those for chlamydia and rates have been highest in the 20-29-year age group. Rates are lower in the 15-19-year and 30-49 year age groups and are noticeably lower in the 50-64-year age group (Figure 4). This is consistent with trends seen elsewhere in Canada.4
As for chlamydial infection, 2018 saw a sharp increase in the rate of reported gonorrhea among 20-29-year-olds. The cause is uncertain, though the fact that chlamydia and gonorrhea rates have both increased in the same age group, in the same year, suggests that increased testing may play a role.
Figure 4: Age-Specific Rates of Gonorrhea, Wellington-Dufferin-Guelph, 2014-2018
Rates by Gender (2014-2018):
The number of cases of gonorrhea in males has consistently been higher than the number of cases in females over the past five (5) years (2014-2018). In four (4) of five (5) years, males accounted for over 60% of reported cases of gonorrhea in WDG (with less than 40% in females). This trend is opposite to that seen for chlamydia, where females account for most of the cases.
The tendency for more cases to be males is consistent with trends reported nationally for gonorrhea.7 This may be partly explained by the greater likelihood that males will have symptoms, seek health care and be tested. In other parts of the world, higher gonorrhea rates are also seen within communities of men who have sex with men (MSM).4
Infectious Syphilis
Syphilis is a bacterial infection spread through vaginal, anal or oral sex. Syphilis can also be transmitted “vertically” from an infected mother to her child during pregnancy or birth.8 Syphilis infections progress through multiple stages, each with their own symptoms, though early symptoms include genital sores, rash and headache.9 Later stages of syphilis can affect the brain, heart, or other organs.9 Spread of syphilis can be prevented through condom use, testing/treatment and routine screening for pregnant women.
Key findings from local data reveal that:
- There are a small number of syphilis cases in WDG, making it difficult to draw conclusions about trends;
- Rates in WDG are lower than provincial rates;
- Rates were highest in the 20-29-year age group, but older adults account for a greater share of infections than they did for chlamydia or gonorrhea; and
- Males accounted for more reported cases than females.
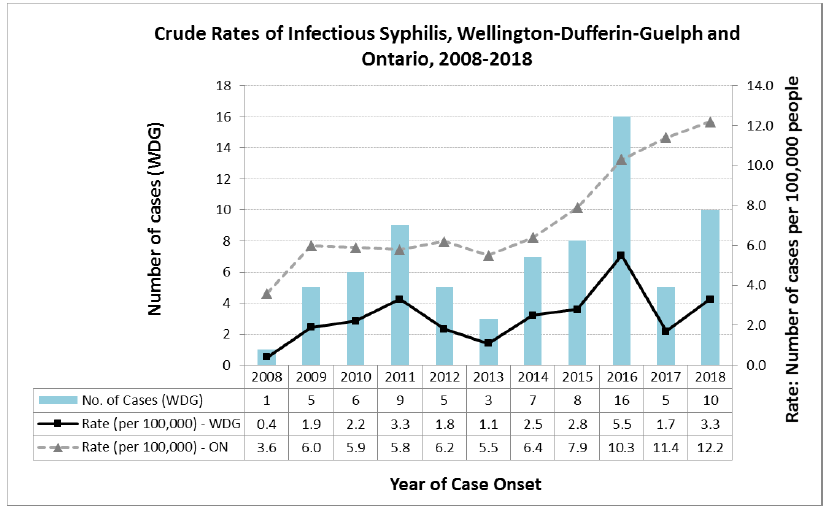
Trends over Time (2008-2018):
Infectious syphilis was the least commonly reported STI in WDG. While rates have been increasing in Ontario over the past decade, there is not clear evidence of an increase in WDG. Small numbers of reported cases (fewer than ten in most years) limit the reliability of trends in the data, so this data should be interpreted with some caution. The rate in WDG was consistently lower than the provincial rate during this time (Figure 5). Adjustments to account for age differences between the WDG and Ontario populations do not significantly change these rates.
Figure 5: Crude Rates of Infection Syphilis, Wellington-Dufferin-Guelph and Ontario, 2008-2018
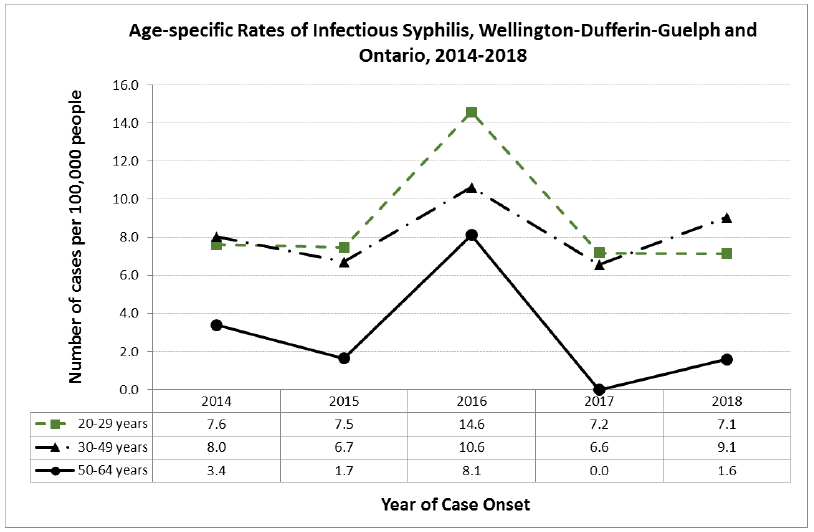
Rates by Age (2014-2018):
Compared to chlamydia and gonorrhea, cases for infectious syphilis tended to be older. Infections were still most common in the 20-29-year age group, though the 50-64-year age group accounted for an important fraction of cases (Figure 6). This is similar to what is seen nationally and likely reflects transmission within MSM communities.4
Figure 6: Age-specific Rates of Infectious Syphilis, Wellington-Dufferin-Guelph and Ontario, 2014-2018
Rates by gender: 2014-2018:
The vast majority of cases of laboratory confirmed infectious syphilis reported in WDG over the past five (5) years have been in males. In 2014 and 2015, all cases were in males, while in 2016, 2017 and 2018 about 90% of cases were in males. This is similar to what is seen nationally and likely reflects transmission within MSM communities.4
Sexual Practices in WDG
Lack of condom use is a risk factor for STIs.10 Data from the Canadian Community Health Survey (CCHS) conducted by Statistics Canada showed that in 2014, 28.3% of WDG respondents and 32.7% of Ontario respondents said that they had not used a condom when they had last had sex. In 2016, these percentages were 72.9% and 62.9%, respectively.11 This indicates a rising trend in this unsafe sexual practice, which is reflected in data collected during WDGPH STI case follow-up interviews.
Having multiple sexual partners is another recognized risk factor for STIs.10 In the 2012 CCHS, 16.0% of sexually active males and 9.9% of sexually active females in WDG reported having had more than one (1) sexual partner in the past 12 months. In 2016, these percentages decreased to 6.8% of males and 8.3% of females. Provincially, the proportion of sexually active males and females reporting more than one sexual partner in the past 12 months also decreased between the 2012 and 2016 surveys.11 This appears to show a relatively recent decrease in the percentage of the population with more than one (1) partner in a year for both males and females. However, it remains to be seen whether this trend will continue.
Conclusion
Both chlamydia and gonorrhea cases are on the rise in WDG and multiple factors are likely contributing to this increase. Based on the data, lack of condom use, multiple or new sexual partners within six (6) months of diagnoses and sex with the opposite sex are the majority of risk factors associated with these infections. Despite recommendations for annual chlamydia and gonorrhea screening, many people are not tested and therefore don’t know they are infected, increasing the spread of diseases.12 Additionally, middle-aged and older adults are re-entering the dating scene and may not know they should or how to get tested for sexually transmitted infections.13 Finally, diseases such as Human Immunodeficiency Virus (HIV) and Acquired Immunodeficiency Syndrome (AIDs) are considered a chronic and manageable disease in some populations reducing condom use in these populations.13
In all WDGPH offices, the Clinical Services team provides sexual health services including: sexually-transmitted infections (STI) testing & treatment; risk counselling; contraception; point-of-care HIV testing; and harm reduction services.
Screening for STIs is offered through Outreach Services at several community partners including: ARCH (HIV/AIDS Resources & Community Health); Community Health Van (in partnership with ARCH & Sanguen Health); Hope House; Wyndham House Resource Centre; Community Health Centre in Guelph; and the University of Guelph. Screening for STIs is also provided at special community events in conjunction with community partners.
Education, public awareness campaigns and increased access to testing are all strategies that WDGPH can use to help detect and treat sexually transmitted infections such as chlamydia and gonorrhea. Additional surveillance and assessment is required to further understand the increase in these infections moving forward.
Ontario Public Health Standard
Sexual Health, Sexually Transmitted Infections, and Blood-borne Infections (including HIV):
in Reported Sexually Transmitted Infections in Wellington-Dufferin-Guelph BH.01.MAY0119.R13 11 of 13
- To prevent or reduce the burden of sexually transmitted infections and blood-borne infections.
Population Health Assessment and Surveillance:
- To provide direction on population health assessment and surveillance activities as defined in the Standards to ensure that local public health practice is informed to effectively and efficiently identify and address current and evolving population health issues.
WDGPH Strategic Direction(s)
✓ Health Equity: We will provide programs and services that integrate health equity principles to reduce or eliminate health differences between population groups.
Organizational Capacity: We will improve our capacity to effectively deliver public health programs and services.
✓ Service Centred Approach: We are committed to providing excellent service to anyone interacting with WDG Public Health.
✓ Building Healthy Communities: We will work with communities to support the health and well-being of everyone.
Health Equity
The information provided in this report shows that some sections of the local population are affected by STIs more than others, with higher incidence of the infections in particular age groups, and with cases of infectious syphilis disproportionately affecting the MSM community.
Public Health can attempt to address these inequities by targeting educational activities and provision of resources at the sections of the population at higher-risk for sexual practices associated with transmission of STIs and with higher incidence rates of lab-confirmed STIs as reflected by surveillance data.
References
1. Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2017. Atlanta: U.S. Department of Health and Human Services; 2018 [cited 2019 Feb 7]. Available from: https://www.cdc.gov/std/stats17/2017-STD-Surveillance-Report_CDC-clearan….
2. Public Health Ontario. Chlamydia [Internet]. Toronto: Government of Ontario; 2019 [cited 22 Apr 2019]. Available from: https://www.publichealthontario.ca/en/diseases-and-conditions/infectious….
3. Public Health Agency of Canada. Canadian Guidelines on Sexually Transmitted Infections – Management and treatment of specific infections – Chlamydial Infections [Internet]. Ottawa: Government of Canada; 2010 [cited 2019 Apr 22]. Available from: https://www.canada.ca/en/public-health/services/infectious-diseases/sexu….
4. Public Health Agency of Canada. Report on Sexually Transmitted Infections in Canada: 2013-2014. Ottawa: Government of Canada; 2017 [cited 2019 Apr 17]. Available from: https://www.canada.ca/en/public-health/services/publications/diseases-co….
5. Public Health Ontario. Gonorrhea [Internet]. Toronto: Government of Ontario; 2019 [cited 22 Apr 2019]. Available from: https://www.publichealthontario.ca/en/diseases-and-conditions/infectious….
6. Public Health Agency of Canada. Canadian Guidelines on Sexually Transmitted Infections – Management and treatment of specific infections – Gonococcal Infections [Internet]. Ottawa: Government of Canada; 2013 [cited 2019 Apr 22]. Available from: https://www.canada.ca/en/public-health/services/infectious-diseases/sexu….
7. Choudhri Y, Miller J, Sandhu J, Leon A, Aho J. Gonorrhea in Canada, 2010-2015. Can Commun Dis Rep. 2018 Feb;44(2):37-42 [cited 2019 Feb 14]. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5933854/.
8. Public Health Ontario. Syphilis [Internet]. Toronto: Government of Ontario; 2019 [cited 22 Apr 2019]. Available from: https://www.publichealthontario.ca/en/diseases-and-conditions/infectious….
9. Public Health Agency of Canada. Canadian Guidelines on Sexually Transmitted Infections- Management and treatment of specific infections – Syphilis [Internet]. Ottawa: Government of Canada; 2010 [cited 2019 Apr 22]. Available from: https://www.canada.ca/en/public-health/services/infectious-diseases/sexu….
10. Public Health Agency of Canada. Canadian Guidelines on Sexually Transmitted Infections – Primary care and sexually transmitted infections [Internet]. Ottawa: Government of Canada; 2013 [cited 2019 Apr 22]. Available from: https://www.canada.ca/en/public-health/services/infectious-diseases/sexu….
11. Statistics Canada, Canadian Community Health Survey, 2014 /2016.
12. Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2014 [Internet]. 2019 [cited April 23, 2019]. Available from: http://www.cdc.gov/nchhstp/newsroom/2015/std-surveillance-report-press-r….
13. M - Relich S, Taylor M, Konkin K. Chlamydia, gonorrhea and syphilis on the rise: Is Tinder to blame? [Internet]. 2016 Jun 9 [cited April 23, 2019]. Available from: http://healthydebate.ca/2016/06/topic/chlamydia-gonorrhea-rise-tinder-blame
Appendices
n/a.