Meeting Date: May 1, 2019
Report No. BH.01.MAY0119.R12
Prepared By: Karen Mulvey, Interim Manager, Clinical Services
Approved By: Rita Isley, Director, Community Health
Submitted By & Signature: Dr. Nicola J. Mercer, MD, MBA, MPH, FRCPC Medical Officer of Health & CEO
Recommendations
It is recommended that the Board of Health:
- Receive this report for information.
- Send a letter to the Minister of Health and Long-Term Care requesting that Emergency Medical Service (EMS) organizations be listed as eligible community organizations that are permitted to distribute naloxone kits to eligible individuals in the community.
Key Points
- Opioid overdoses are an important cause of death, in Ontario, and locally in Wellington, Dufferin and Guelph (WDG). The rate of opioid-related deaths in WDG has increased 420 percent since 2005 and has nearly tripled in the past three (3) years (from 8 deaths in 2015 to 23 deaths in 2017).
- Take-home naloxone programs, in which people at-risk of overdose are provided with naloxone kits and training, are effective at decreasing rates of opioid-related deaths.
- Wellington-Dufferin-Guelph Public Health (WDGPH) provides free naloxone kits to individuals in the community and supplies kits to eligible community organizations to distribute further. In 2018, WDGPH and 16 community organizations distributed 1,419 naloxone kits in the community.
- Currently, Emergency Medical Service (EMS) organizations are not eligible to distribute naloxone kits as part of the Ontario Naloxone Program. Given the contact that first responders have with people at-risk of overdose, distribution of kits by EMS organizations would expand the reach of the naloxone program.
Discussion
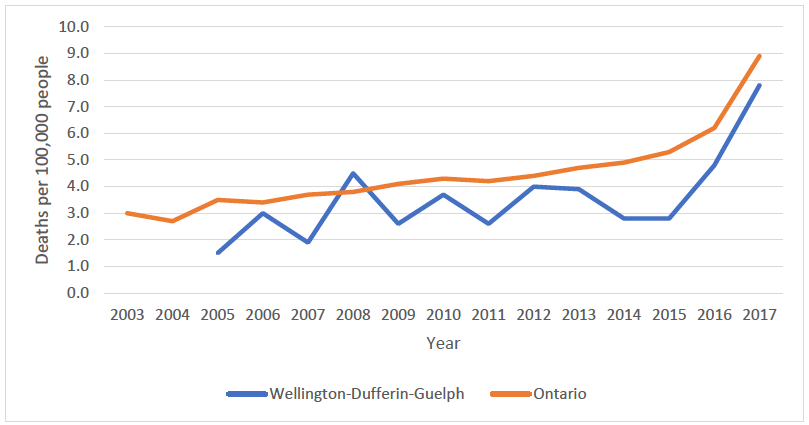
Opioids remain a leading cause of death in Ontario. From 2003-2017, the rate of opioid-related deaths (mortality rate) has increased 197 percent. There were over 1,250 opioid-related deaths in 2017.1
Opioid-related mortality has also increased in WDG during this same period of time. Though rates of opioid-related deaths have been lower locally in WDG, than Ontario, they have increased 420 percent since 2005. This increase was more pronounced during the most recent three (3) years for which data is available (2015-2017), during which time the rate of opioid-related deaths nearly tripled (Figure 1).1
Figure 1: Rates of opioid-related deaths in Wellington-Dufferin-Guelph and Ontario, 2003-2017.1
Opioid overdoses can result in death as the drug affects a person’s natural ability to breath which leads to decreased delivery of oxygen to vital organs such as the brain and heart.2 Naloxone is a medication that can reverse the effects of an opioid overdose and is available as an injection or nasal spray.2 Take-home naloxone programs, in which people at-risk of overdose are provided with naloxone kits and training, are effective at decreasing rates of opioid-related deaths.3
Figure 2: Programs providing publicly-funded naloxone kits in Ontario.4
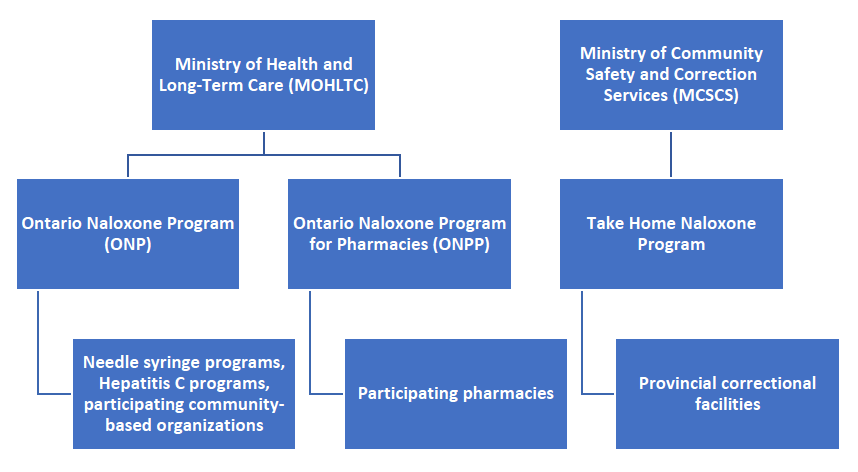
In Ontario, naloxone kits are available at pharmacies, provincial correctional facilities and some community-based organizations.4 In early 2017, WDGPH began working with AIDS/HIV Resources & Community Health (ARCH) to distribute free nasal naloxone to people who meet Ministry of Health and Long-Term Care (MOHLTC) criteria (individual opioid users, their friends/family and recently released inmates). In September 2017, the MOHLTC introduced the Harm Reduction Program Enhancement and tasked public health units with distributing naloxone kits through eligible community organizations including: Community Health Centres (including Aboriginal Health Access Centres); AIDS Service Organizations; Shelters; Withdrawal Management Programs; and Outreach Programs.5 In 2018, the program expanded to include: hospitals; police; fire services; and St. John Ambulance branches.4 Public health units provide naloxone kits to these organizations, which in turn offer them to clients who meet MOHLTC criteria.
WDGPH enrolled 16 community organizations in the Naloxone Distribution program in 2018, compared to seven in 2017. Each participating organization receives:
- A one-hour training session with a Public Health Nurse prior to enrollment, which uses a ‘train-the-trainer’ model to ensure that the organization’s staff/volunteers are able to teach clients how to recognize an overdose and use naloxone properly;
- Support to develop administrative practices (e.g. policies and procedures) to facilitate naloxone distribution and reporting;
- Naloxone kits based on their self-identified needs; and
- Each organization is invited to an annual meeting to review community processes and data collection related to naloxone kit distribution.
In conjunction with community organizations, WDGPH distributes naloxone kits to individuals, at all of its offices, through the Stay Sharp program and the Community Outreach Van. In 2018, WDGPH, in conjunction with community partners, distributed 1,419 naloxone kits to individuals in WDG. This number does not include kits distributed by pharmacies or the Sanguen Health Centre.
Conclusion
The Naloxone Distribution Program contributes to WDGPH’s harm reduction initiatives and provides direct services to people who use substances. This life saving measure supports the MOHLTC’s Harm Reduction Initiative as opioid-related harms continue to rise in the province of Ontario.
Currently, EMS organizations are not on the list of community organizations who can distribute naloxone to individuals. Though EMS first responders are able to administer naloxone, in an emergency scenario, they are not permitted to provide naloxone kits to individuals at-risk of overdose who choose not to go to the hospital. The contact that EMS first responders have with opioid users could provide another opportunity for naloxone kits to be given to individuals in need – similar to the rationale by which hospital emergency departments distribute naloxone. The list of community agencies that can distribute naloxone through the Ontario Naloxone Program is determined provincially by the MOHLTC.
Naloxone distribution is an evidence-based, harm reduction initiative that prevents overdose deaths in the WDG community. WDGPH will continue to explore new ways to expand the reach of this program.
Ontario Public Health Standard
Substance Use and Injury Prevention
Goal: To reduce the burden of preventable injuries and substance use.
Requirements:
- The board of health shall develop and implement a program of public health interventions using a comprehensive health promotion approach that addresses risk and protective factors to reduce the burden of preventable injuries and substance use in the health unit population.
Infectious and Communicable Disease Prevention and Control
Goal: To reduce the burden of communicable diseases and other infectious diseases of public health significance.
Requirements:
- The board of health shall collaborate with health care providers and other relevant partners to ensure access to, or provide based on local assessment, harm reduction programs in accordance with the Substance Use Prevention and Harm Reduction Guideline, 2018 (or as current).
WDGPH Strategic Direction(s)
✓ Health Equity: We will provide programs and services that integrate health equity principles to reduce or eliminate health differences between population groups.
Organizational Capacity: We will improve our capacity to effectively deliver public health programs and services.
✓ Service Centred Approach: We are committed to providing excellent service to anyone interacting with WDG Public Health.
✓ Building Healthy Communities: We will work with communities to support the health and well-being of everyone.
Health Equity
Reducing health differences between populations is the essence of health equity and is a key direction in WDGPH’s strategic plan.
The Naloxone Distribution Program works very closely with community partners to implement this potentially life-saving intervention for people who use substances. Community partners involved in naloxone distribution are in a unique position to provide access to those who would otherwise face barriers to this service.
Increasing access to naloxone broadly across the community will assist the most marginalized populations with accessing this lifesaving medication. Often substance users shy away from accessing main stream services due to the stigma attached to their illness and how the general public reacts. Providing access where the individuals reside reduces these barriers and the stigma associated with the illness.
References
1. Public Health Ontario. Interactive Opioid Tool [Internet]. 2019. Available from https://www.publichealthontario.ca/en/data-and-analysis/substance-use/in….
2. Harm Reduction Coalition. What is an overdose? [2019]. Available from: https://harmreduction.org/issues/overdose-prevention/overview/overdose-b…
3. Wellington Dufferin Guelph Board of Health. BOH report-BH.01.Oct0318.R31-Opioid Harm Reduction Update in Wellington Dufferin and Guelph [Internet]. 2018 Oct 03. Available from: https://www.wdgpublichealth.ca/board-health/board-health-reports
4. Ministry of Health and Long-Term Care. Naloxone: Frequently Asked Questions. 2019. [Internet]. 2019 [cited April 23, 2019]. Available from: http://www.health.gov.on.ca/en/pro/programs/drugs/naloxone/naloxone_faq….
5. Ministry of Health and Long-Term Care. Harm Reduction Program Enhancement Questions and Answers. 2017. [Internet]. 2019 [cited April 23, 2019]. Available from: http://eenet.ca/sites/default/files/2018/January/Harm%20Reduction%20Prog…
Appendices
None.