Meeting date: October 3, 2018
Prepared by: Kyley Alderson, Health Promotion Specialist, Chronic Diseases Prevention; Michael Whyte, Health Promotion Specialist, Health Analytics,;Amy Estill, Manager, Chronic Diseases Prevention; Jennifer Macleod, Manager, Health Analytics
Report no.: BH.01.OCT0318.R31
Approved by: Rita Isley, Director, Community Health & Wellness
Submitted by: Dr. Nicola J. Mercer, MD, MBA, MPH, FRCPC, Medical Officer of Health and CEO
Recommendations
It is recommended that the Board of Health:
- Receive this report for information.
Key Points
- Within the past five (5) years, Emergency Department (ED) visits and mortality due to opioids has been steadily increasing in Wellington County, Dufferin County, and the City of Guelph (WDG).
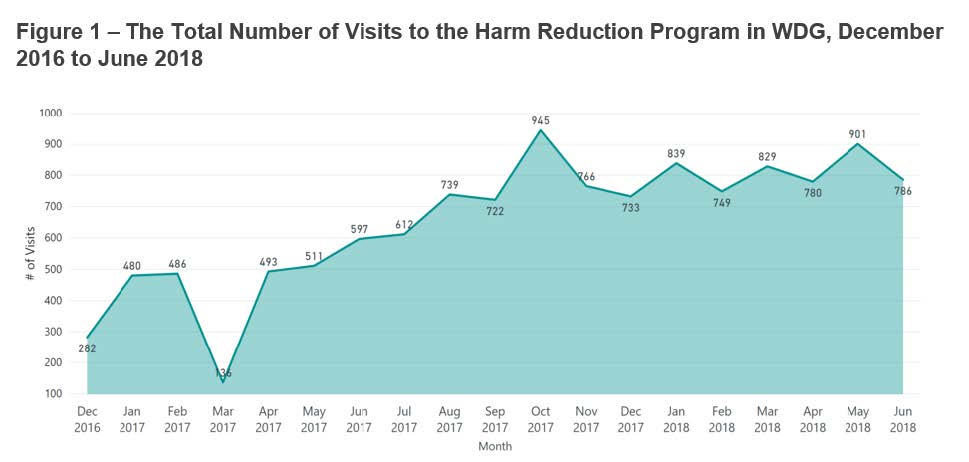
- The use of harm reduction services has continued to increase since December 2016 under the Harm Reduction Program with Wellington-Dufferin-Guelph Public Health (WDGPH) and community partners.
- WDGPH continues to expand the distribution of free nasal naloxone to organizations under the Naloxone Distribution Program.
- Interviews conducted in downtown Guelph with people who use illicit substances revealed that participants were scared about overdose and dying, and that there was strong support among this group for a supervised consumption site. In addition, many participants were facing complex challenges in their lives, which are important to consider in a community approach to reduce substance use harm.
- The first Overdose Prevention Site (OPS) in the City of Guelph opened in May 2018. During the first four months of operation, the OPS had 1363 visits to the service. Within this time, there were 14 opioid overdoses, and all were successfully reversed.
- Next steps underway for harm reduction activities at WDGPH include phase 2 of the substance use needs assessment, an expansion of harm reduction services, and the launch of a harm reduction campaign.
- Harm reduction and Overdose Prevention Sites are an integral part of a comprehensive strategy to reduce the negative impact that opioids have in the community.
Discussion
Background
Within the past five (5) years, ED visits and mortality due to opioids have been steadily increasing in Ontario and WDG. In 2017, the rate of opioid-related ED visits reached 54.6 visits per 100,000 residents across WDG.1 Consistent with the rise in ED visits, opioid-related mortality in 2017 was 8.1 per 100,000 in WDG, approximately three (3) times higher than the rate in 2015.2
WDGPH and community partners are responding to opioid and other substance related harms in the community through a variety of strategies. This report provides an update on the harm reduction programs and services within WDG.
Public Health and Community Responses to the Opioid-Related Harms
Harm Reduction Program
Under the Harm Reduction Program, WDGPH continues to distribute unused needles, crack pipes and other drug paraphernalia to the community in partnership with AIDS/HIV Resources & Community Health (ARCH) and Sanguen Health Centre. Collection and disposal of used supplies, counseling services and referrals are also offered under this program.
The use of harm reduction services has been increasing since December 2016 (Figure 1).
Visit information includes numbers from three service providers:
- ARCH - an AIDS/HIV service organization with several locations around Guelph.
- Public Health – services delivered from both the Chancellors Way and Orangeville WDGPH offices.
- Community Health Van (CHV) – a mobile harm reduction service coordinated by WDGPH and Sanguen Health Centre. Beginning in October 2017, the CHV began distributing harm reduction supplies to several locations around the City of Guelph every Wednesday and Thursday nights.
Figure 1 - The Total Number of Visits to the Harm Reduction Program in WDG, December 2016 to June 2018
Naloxone Distribution Program
In June of 2017, the Ministry of Health and Long-Term Care (MOHLTC) announced that it would provide local health units with additional funding to increase their capacity for harm reduction services. A portion of this funding is dedicated toward naloxone distribution and training of local partners and priority populations. The details of the program have been described in Board of Health (BOH) Report BH.01.MAY0218.R13.3
Since the May BOH report, WDGPH has collaborated with police services and local hospitals, to make naloxone available to prevent overdoses in their daily work. Currently, eleven (11) organizations have finalized their agreement to distribute naloxone through the MOHLTC program and three (3) organizations are currently undergoing the process of becoming eligible to distribute Naloxone under the Ontario Naloxone Program.
Needs Assessment Phase I: Interviews with people who use substances in downtown Guelph
Interviews were conducted in April 2018 with people who use illicit substances to help community organizations better understand substance use behaviours and identify the needs of people who use substances in Guelph. An advisory committee consisting of representatives from WDGPH, Wellington Guelph Drug Strategy, ARCH, Sanguen Health Centre and Toward Common Ground oversaw the project. The interviews were conducted by a trained peer researcher (someone with lived experience of substance use) and participants were recruited at a variety of locations in downtown Guelph, including: Guelph Community Health Centre, Royal City Church, Welcome In Drop In, Hope House, OATC and Wyndham House Resource Centre. These locations were chosen in consultation with the committee to enhance opportunities for participation (i.e., reaching people who use different services) and to efficiently meet timelines (i.e., ensuring eligible participants).
Of the 108 people interviewed, crystal meth was the most commonly used substance (used by 58% of participants), followed closely by opioids (49%). Smoking (54%) and injection (47%) were the most common methods of consuming substances. Participants used substances in a mix of public and private locations, the five (5) most common being their own place (68%), a relative or friend’s place (58%), a public washroom or toilet (51%), a hotel or motel (37%), and in a stairwell or doorway (36%).
The majority of participants reported that their biggest fears and worries around substance use were overdose or dying (62%). Numerous people reported that they had already lost family members and friends and many were concerned about the contamination of the drug supply. The majority of participants (55%) had experienced an adverse reaction to using substances. Reactions varied, but the most common symptom reported was unconsciousness or not being able to remember the event. In many cases, the participant reported going to the hospital and/or that naloxone was used. The majority of these adverse reactions were attributed to opioids. In some cases, fentanyl was purposely being used, but in others, the substance was much stronger than they anticipated or it was suspected of being contaminated with fentanyl. In six (6) individuals who reported an adverse event, a suicide attempt was identified.
There was strong support among participants for a supervised consumption site in the community. When participants were asked about what they would like to see in Guelph to help them be safe while using, 40% said a safe place where they could use substances, such as a supervised injection site. When participants were asked directly about whether they would go to a safe place where they could legally use substances, 83% of people said they would, 15% said they wouldn’t, and 2% were unsure. In May of this year, shortly after these responses were collected, an Overdose Prevention Site was opened in downtown Guelph. For more information, see the ‘Overdose Prevention Site’ section below.
Many participants thought the current services in Guelph were good, but that an expansion of existing services, especially Stay Sharp Needle Exchange (hours of operation, locations, and needle drop boxes) would be helpful. More counsellors to talk to, and the need for 24/7 services and programs were also themes among participants.
These interviews revealed that participants were facing complex challenges in their lives. Many participants did not have their basic needs met, such as shelter/housing and access to food. Many participants reported a need for counselling, financial support, mental health support, primary health care, pain management, employment opportunities, detox, recreation/leisure opportunities and access to transportation. Some participants were not aware of all the services currently offered in the community and others reported barriers to accessing existing community services, such as waiting lists, difficulties in keeping appointments or making required phone calls (especially without having a phone), or hours of operation. An understanding of underlying or co-morbid factors, and a consideration for the unique challenges people face in accessing appropriate support, are essential in any community approach to reduce substance use harm.
An important limitation of these interviews are that findings are not generalizable to all people who use substances in the community. Recruitment only took place in downtown Guelph, so likely did not include individuals who live or spend time elsewhere. People who were not accessing services at recruitment locations were also less likely to be included, although word of mouth recruitment and promotion did recruit some people who may not traditionally access those services.
Nevertheless, these findings provide community organizations with a richer understanding of substance use behaviours and community needs among participants. Involving peer researchers in the planning, recruitment and interview process contributed to high quality data, including appropriate interpretation of questions and open and honest responses.
Findings are being shared back with people who use substances in the community, as well as service providers, funders and other community stakeholders and decision makers. This information will help to support evidence-based decision-making regarding community programs and services in Guelph. Appendix “A” contains additional interview findings.
Overdose Prevention Site (OPS)
In May 2018, WDG’s first Overdose Prevention Site opened in the City of Guelph. This service, which is staffed by a Registered Nurse and Peer Worker, includes two (2) consumption booths where staff provide medical supervision, assessment and monitoring for individuals to consume pre-obtained substances. This service is designed to reduce the number of opioid-related overdose deaths; and also offers needle exchange services, access to naloxone, health teaching and counselling, wound care, and referrals to other health and social services, including addiction treatment and withdrawal management. There is space for quiet activities, allowing staff more time to monitor for adverse reactions. Although WDGPH is not a key partner in the development and sustained operation of the OPS, the health unit is participating in a lead role in evaluating the sites’ operations.
Within the first four (4) months of operation (May to August 2018), the OPS has had 1,363 visits. The service is used by 181 unique people and opioids were used in 75% of visits. There were 14 opioid overdose reversals in four (4) months, with seven (7) occurring in the month of August. Every overdose was successfully reversed using oxygen and/or naloxone.
Next Steps
Reducing harms from substance use in the community requires a comprehensive strategy that reaches different population groups across the WDGPH geography. This type of strategy requires partnerships that span health and social services sectors, government, and private businesses. In order to effectively reduce harms, the strategy must be tailored to meet the needs of people who use substances in WDG.
1) Needs Assessment
Phase II of the substance use needs assessment will take place in the fall of 2018. Whereas recruitment for Phase I of the needs assessment targeted people who were connected to services in downtown Guelph, Phase II of the needs assessment aims to encourage participation from people who use illicit substances in WDG. This will be accomplished through an online survey that will be heavily promoted online and in local organizations. The primary goals of the needs assessment are to:
- Increase our understanding of substance use behaviors;
- Identify gaps in services and programs;
- Determine the potential role of a SCS; and
- Explore the need and sustainability for other harm reduction programs and services.
The information from the Phase II Needs Assessment will be used internally and shared with community partners and members of government to inform planning of programs and services to reduce harms from substance use.
2) Harm Reduction Services
Under the Harm Reduction Program, harm reduction services are distributed through several locations within the City of Guelph. The program also delivers harm reduction services through the Fergus and Orangeville WDGPH offices. In the Fall of this year, harm reduction services will be extended into the rest of Wellington County through the CHV to improve access across WDG. WDGPH is continuing to look for opportunities to expand services and collaborate with partners in areas of Dufferin County to improve access to services for all areas of WDG.
3) Harm Reduction Campaign
WDGPH is working in partnership with local community organizations to develop a harm reduction focused awareness campaign that will be released in the fall of 2018. The campaign aims to raise awareness among the general public about substance use harm reduction practices. The campaign will be distributed widely across WDG using various communication channels. This distribution plan will allow WDGPH to reach people who use substances who typically do not access harm reduction messaging through traditional programs and services due to barriers like transportation, stigma, or infrequent use. The campaign will provide harm reduction messaging in an accessible and de-stigmatizing format to encourage all individuals to seek resources to reduce their risk of harm from substance use.
Conclusion
Opioid-related harms are a growing concern across the province. WDGPH is currently working to identify and implement a comprehensive strategy to deliver harm reduction services to people who use substances.
Ontario Public Health Standard
Foundational Standards:
Health Equity
Goal: Public health practice results in decreased health inequities such that everyone has equal opportunities for optimal health and can attain their full health potential without disadvantage due to social position or other socially determined circumstances.
Effective Public Health Practice
Goal: Public health practice is transparent, responsive to current and emerging evidence, and emphasizes continuous quality improvement.
Program Standards:
Substance Use and Injury Prevention
Goal: To reduce the burden of preventable injuries and substance use
Requirements:
- The board of health shall collect and analyze relevant data to monitor trends overtime, emerging trends, priorities, and health inequities related to injuries and substance use and report and disseminate the data and information in accordance with the Population Health Assessment and Surveillance Protocol,2018 (or as current).
- The board of health shall develop and implement a program of public health interventions using a comprehensive health promotion approach that addresses risk and protective factors to reduce the burden of preventable injuries and substance use in the health unit population.
Infectious and Communicable Diseases Prevention and Control
Goal: To reduce the burden of communicable diseases and other infectious diseases of public health significance.
Requirements:
- The board of health shall collaborate with health care providers and other relevant partners to ensure access to, or provide based on local assessment, harm reduction programs in accordance with the Substance Use Prevention and Harm Reduction Guideline, 2018 (or as current).
WDGPH Strategic Direction(s)
✓ Health Equity: We will provide programs and services that integrate health equity principles to reduce or eliminate health differences between population groups.
Organizational Capacity: We will improve our capacity to effectively deliver public health programs and services.
✓ Service Centred Approach: We are committed to providing excellent service to anyone interacting with WDG Public Health.
✓ Building Healthy Communities: We will work with communities to support the health and well-being of everyone.
Health Equity
Health equity principles are being applied across all WDGPH opioid projects with the goal of reducing or eliminating differences in opioid-related harms between population groups. According to a study by the Public Health Agency of Canada, opioid and other drug-related overdose deaths occurred across all sociodemographic and socioeconomic groups. However, characteristics most common among those who died include4:
- a history of mental health concerns, substance use disorder, trauma, and stigma
- decreased drug tolerance
- being alone at the time of overdose
- lack of social support
- lack of comprehensive and coordinated healthcare and social service follow-up
Supervised Consumption Sites tend to engage people who are more socially marginalized, such as people experiencing unstable living arrangements or homelessness, mental health concerns and/or chronic substance use.5 Different approaches and strategies are needed to reach a diversity of groups who have different risk factors and different needs. WDGPH will continue to explore the needs of different population groups and use a comprehensive and targeted approach to reduce health inequities and reduce the burden of substance related harm in the community.
References
1. National Ambulatory Care Reporting System (NACRS). 2003-2017, Ontario Ministry of Health and Long Term Care, IntelliHEALTH Ontario; accessed 23 Aug 2018.
2. Ontario Opioid-Related Death Database, 2005-2017, Office of the Chief Coroner for Ontario; accessed through the Interactive Opioid Tool 31 Aug 2018.
3. Wellington-Dufferin-Guelph Board of Health. BOH report – BH.01.MAY0218.R13 Naloxone Distribution Program. [Internet]. 2018 May 4. [cited 2018 Sep 24]. Available from: https://www.wdgpublichealth.ca/sites/default/files/file-attachments/BOH/…
4. Special Advisory Committee on the Epidemic of Opioid Overdoses. Highlights from phase one of the national study on opioid- and other drug-related overdose deaths: insights from coroners and medical examiners [Internet]. Public Health Agency of Canada. 2018 Sept [cited: 2018 Sept 24]. Available from: https://www.canada.ca/en/public-health/services/publications/healthy-liv…
5. Wellington-Dufferin-Guelph Board of Health. BOH report - BH.01.MAR0718.R06 Community Response to Opioid Harms: Considerations for Supervised Consumption Sites. [Internet]. 2018 Mar 7. [cited 2018 Sep 24]. Available from: https://www.wdgpublichealth.ca/sites/default/files/file-attachments/basi…
Appendices
Appendix “A” - Needs Assessment Phase 1 – Interviews with people who use substances in downtown Guelph: Summary of Key Findings
Appendix “A”
Needs Assessment Phase 1 – Interviews with people who use substances in downtown Guelph: Summary of Key Findings
Demographics
| Sex | # | % |
|---|---|---|
| Male | 69 | 64 |
| Female | 38 | 35 |
| Non-Binary | * | * |
Substance Use Behaviours and Harms
| Substance Used | % |
|---|---|
| Cystal Meth | 58 |
| Opioids1 | 49 |
| Cocaine2 | 24 |
| Party Drugs/Hallucinogens | 6 |
| Benzodiazepines | 3 |
| Frequency of Use | % |
|---|---|
| Everyday | 64 |
| At least once a week | 21 |
| At least once a month | 7 |
| Less than once every month | 5 |
| Have not used in past 6 months* | 3 |
| Method of Use | % |
|---|---|
| Smoked | 54 |
| Injected | 47 |
| Snorted | 29 |
| Eat/Swallowed | 19 |
| Top 5 Locations of Use3 | % |
|---|---|
| Own Residence | 68 |
| Relative or friends place | 58 |
| Public Washroom/Toilet | 51 |
| Hotel/Motel | 37 |
| Stairwell/Doorway | 36 |
| Ever experienced an adverse reation4 | % |
|---|---|
| Yes | 55 |
| No | 45 |
Use of Existing Services (Past 6 months)
| Use of Existing Services (Past 6 months) | # | % |
|---|---|---|
| Needle Exchange/Harm Reduction Supplies | 78 | 72 |
| Community Health Van | 55 | 51 |
| Naloxone | 49 | 45 |
| SOS/ARCH Outreach | 41 | 38 |
| Emergency Services | 37 | 34 |
| CMHA Here 24/7 | 35 | 32 |
| Methadone Clinic | 33 | 31 |
Supervised Consumption Site (SCS) and Services
| Willing to go to SCS | % |
|---|---|
| Yes | 83 |
| No | 15 |
| Unsure | 2 |
| Top 5 Most Important Services | % |
|---|---|
| Nursing staff | 50 |
| A “chill out” room after using substance | 35 |
| Food (including take-away) | 32 |
| Washrooms | 31 |
| Withdrawl management | 31 |
* Data have been supressed due to cell counts of <5
1Heroin and hydromorphone (including dialudid) were the most commonly used opioids
2Of those who used cocaine, 30% were using crack cocaine
3The timing of year may have influenced locations of use
4Adverse reaction defined as having had a very negative reaction to taking/using too much drugs, losing consciousness, or feeling that life was at risk