The information on this page is reproduced from the booklet Infant Formula: What You Need to Know with permission from the Baby-Friendly Initiative Strategy for Ontario.
This information is also available in different languages on printable fact sheets.
Using this booklet
Families feed formula for medical or personal reasons, exclusively or as a supplement. This resource will help parents, families, caregivers, and childcare providers prepare, feed and store formula safely. The information is meant for healthy, term babies. This booklet includes information about the risks and costs of formula feeding to help families make an informed decision.
This booklet will guide you to:
- Make an informed decision.
- Prepare three types of formula safely.
- Feed your baby according to your baby’s feeding cues.
- Store and transport formula safely
In this booklet, the word “formula” is used. Other names for formula are:
- Artificial baby milk.
- Breast milk substitutes.
- Commercial infant formula.
- Manufactured infant milk.
- Manufactured mother’s milk.
- Non-human milk.
Table of Contents
Supplementing a Breastfed Baby
Cleaning Bottles and Equipment
Sterilizing Bottles and Equipment
Choosing Water to Make Formula
How to Sterilize Water, Choose Formula and Bottle-Feeding Supplies
Preparing Ready-to-feed Liquid Formula
Preparing Concentrated Liquid Formula
Feed According to Your Baby’s Cues
Considering Formula Feeding
The World Health Organization, Health Canada, Dietitians of Canada, and the Canadian Paediatric Society recommend breastfeeding for babies and toddlers, exclusively for the first six months, and sustained for up to two years or longer with appropriate complementary feeding. Parents may give their baby infant formula for a variety of reasons.
Parents may feed their baby formula only, or give some formula and some breast milk. Giving formula may not be their first choice. If you need to supplement your breastfed baby, see page 4.
Parents may feel uncomfortable or guilty about giving their baby formula. If you feel this way, it may be helpful to talk with a health care provider.
If feeding formula is the right decision for you and your baby, it is important to have the information you need to feel comfortable with your plan. If you are hoping to return to breastfeeding, contact your health care provider or a lactation consultant to help put in place plans and supports to achieve this.

It is important that all families, who are thinking about giving their baby formula, have the following information to make an informed decision.
Effect on Health
- Giving formula to a breastfed baby can reduce a mother’s breast milk supply and impact her plan to breastfeed.
- Babies who are not breastfed have a higher risk of ear infections, lung and breathing issues, diarrhea, and Sudden Infant Death Syndrome (SIDS).
- Later in life there are increased health risks such as overweight, obesity, and chronic illnesses like diabetes.
- Mothers who do not breastfeed have a higher risk of health issues like postpartum bleeding, type 2 diabetes, breast cancer and ovarian cancer.
In the early days after introducing formula, mothers may experience full and painful breasts. There are many comfort measures you can discuss with your health care provider, including cold compresses, gentle hand expression and the use of anti-inflammatory pain medications.
Financial Cost
The table shows the average cost of feeding a baby with basic formula for one year. This does not include the cost of bottles, nipples, other feeding equipment, or the cost of preparing and storing formula.
| Type of formula | Cost per year |
|---|---|
| Ready to Feed | $3,360 per year |
| Liquid Concentrate | $1,100 per year |
| Powder | $900 per year |
This is an approximate cost of formula from birth to one year. The cost will be different with time and will depend on where you live. Numbers are based on estimates in three parts of Ontario, in 2014 and 2015.
Quality of Formula
Sometimes things can go wrong while formula is being made in the factory. For example, it may come in contact with bacteria, or it may have missing or wrong ingredients. The Healthy Canadians website lists safety concerns and recall alerts. Compare the lot numbers of your formula cans to the lot numbers on this website. To view this website and sign up for alerts, go to: http://healthycanadians.gc.ca/recall-alert-rappel-avis/index-eng.php.
If you decide to feed your baby formula, this booklet provides the information you need to prepare, store and transport formula, and to feed your baby safely. Please review this booklet and discuss any concerns with your health care provider, nurse, public health nurse, lactation consultant, registered dietitian, or other professional.
Supplementing a Breastfed Baby
If you breastfeed and your baby needs more calories, you will need to give a supplement. The best option is breast milk. This can be expressed by hand and/or by pump.
Giving formula to a breastfed baby can decrease your breast milk supply. Supplementing with formula may lead to ending breastfeeding before you had planned to stop. It can be hard to restart breastfeeding after having stopped.
Here is a list of supplements in order of what to try first if available:
- Your own fresh breast milk, hand expressed and/or pumped.
- Your own breast milk that has been frozen and thawed just before using.
- Pasteurized human milk (breast milk) from a human milk bank. Some milk banks may only have enough milk for babies with special needs such as preterm babies.
- Commercial formula that is cow milk-based.
Most babies who drink formula do best with a cow milk-based formula. Specialized formulas should only be used if your health care provider recommends them. Many parents use a bottle to give a supplement, but this not always the best method of feeding a supplement to a baby. Babies who are fed by bottle may find it harder to breastfeed. You can feed your baby a supplement using one or more of the following methods. With the help of a knowledgeable professional consider a:

- Cup (open cup, not sippy cup) or spoon.
- Lactation aid which uses a tube at your breast.
- Finger feeder with a tube attached to your clean finger.
- More specialized feeding devices.
This booklet has information on bottle-feeding supplies on page 9, and how to bottle feed on page 17.
If you are thinking about using formula, or need to give formula, consider:
- Getting knowledgeable help to maintain your breast milk supply and improve breastfeeding.
- Breastfeeding AND feeding formula as a supplement.
- Feeding expressed breast milk and formula.
Resources to support breastfeeding:
- Services in your community such as a breastfeeding clinic or mother-to-mother support. You can find these at: www.ontariobreastfeeds.ca.
- La Leche League at: www.lllc.ca.
- Your local Public Health Unit at: www.health.gov.on.ca/en/common/system/services/phu/locations.aspx.
- Find a lactation consultant in your area.
- Telehealth Ontario 24/7 breastfeeding support at: 1-866-797-0000
How to Choose Formula
Recommendations for choosing formula:
- Cow milk-based formula is recommended for most babies who get formula. Most formulas have a cow milk-base with added nutrients.
- Soy-based formulas are NOT recommended except for babies with a particular medical condition. Sometimes parents decide to use soy for personal, cultural or religious reasons.
- Do NOT use homemade formulas and do NOT use regular cow milk or other animal milks. These do not have the right amount of nutrients and may be harmful to your baby.
- Follow the exact directions on the package for the amounts of water and formula. Adding extra water to formula to make it thinner, or less water to make it thicker, can be unhealthy and dangerous for your baby.
- Formulas sold as organic, made with prebiotics, probiotics, added DHA fats, or made with “partially broken down” proteins are NOT needed. Research has not proven these to be helpful.
- Formula fed babies need to stay on commercial formula until 9-12 months of age. “Follow-up” formula is NOT needed.
There are three types of formulas:
- Ready-to-feed – no water needed.
- Liquid concentrate – needs to be mixed with sterilized water.
- Powder – needs to be mixed with sterilized water.
Ready-to-feed and liquid concentrate formulas are sterile until the can is opened. Powdered formula is not sterile and may carry harmful bacteria that can make your baby sick.
Babies who have the greatest chance of infections should have sterile liquid formula such as ready-to-feed or liquid concentrate formulas.
Babies who are at the greatest risk of infections from powdered infant formula are those who:
- Are premature.
- Had low birth weight and are under two months of age.
- Have a weakened immune system.
Read the following pages for details on how to prepare and feed formula.
Cleaning Bottles and Equipment
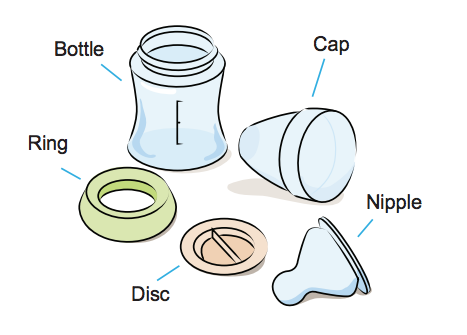
Always clean all bottle and feeding equipment for babies of any age who are being fed formula. This will remove unseen bits of formula or specks of dirt before sterilization.
Use glass bottles or Bisphenol-A (BPA)-free plastic bottles. Make sure all parts have no cracks, are not discoloured and have no loose parts that could break off.
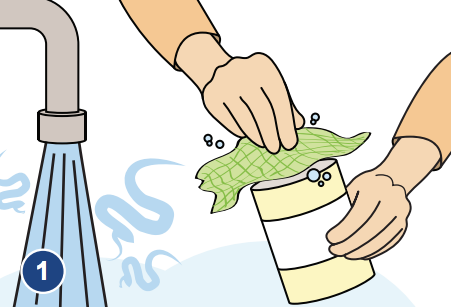
1. Wash your hands
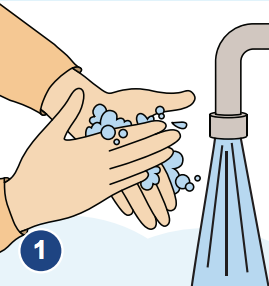
Wash your hands with soap and warm water. Wash your sink and work area with a clean dishcloth, soap and warm water. Then, it is a good idea to sanitize the counter by mixing 5 ml (1 teaspoon) household bleach with 750 mL (3 cups) of water. Put this solution in a spray bottle and label the bottle. Spray your counter and wipe it with a clean towel.
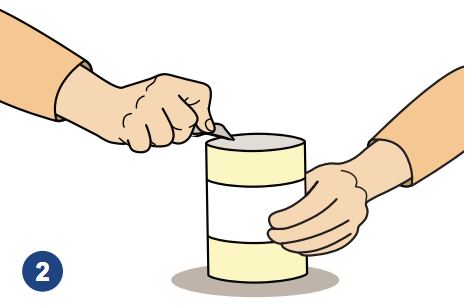
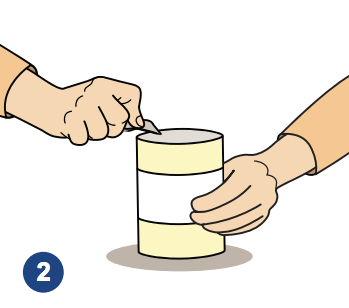
2. Wash equipment
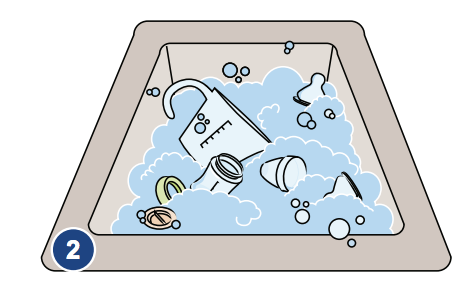
Wash all bottles, nipples, rings, caps, discs, measuring cup, can opener if needed, mixing utensils, and tongs in hot soapy water. If needed also wash containers for storing sterilized water
3. Use a bottle brush
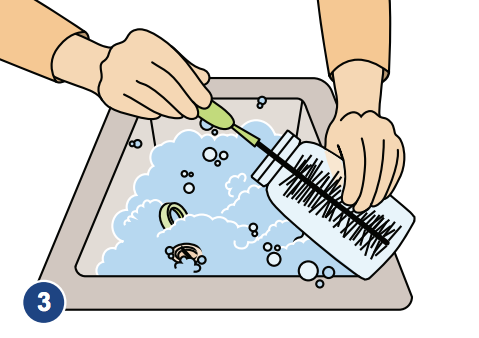
Use a bottle brush that is used only for infant feeding equipment. Scrub inside the bottles and nipples to make sure they are free of any sign of formula.
4. Rinse

Rinse well in hot water. Set the bottles and feeding equipment to air dry on a clean towel, on a clean surface. Now you are ready to sterilize this equipment.
Sterilizing Bottles and Equipment
Sterilize all bottles, feeding equipment, and water for formula for babies of any age. There is no research that says when to safely stop sterilizing. That means it is safest to sterilize water and bottle feeding supplies as long as your baby is drinking formula.
To sterilize the bottles and feeding equipment after washing:
- Fill a large pot with water. Add:
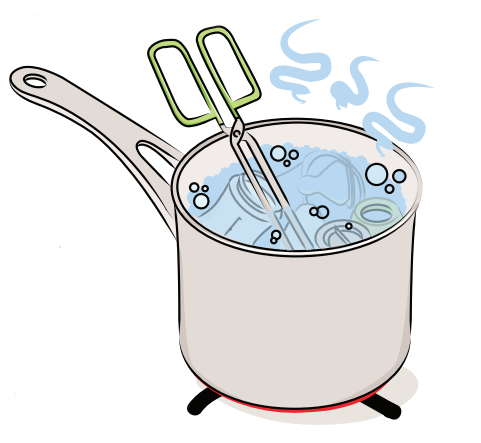
- Bottles.
- Nipples.
- Rings.
- Caps.
- Discs.
- Measuring cup and knife.
- Can opener (if needed), and mixing utensils.
- Tongs with handle sticking out.
- Make sure all your equipment is covered with water and there are no air bubbles.
- Bring the water in the pot to a boil. Let it boil for two minutes, without the lid on.
- Use the sterilized tongs to remove the bottles and feeding equipment from the water. Shake excess water off. Set the equipment to air dry on a clean towel. The equipment is now ready to use.
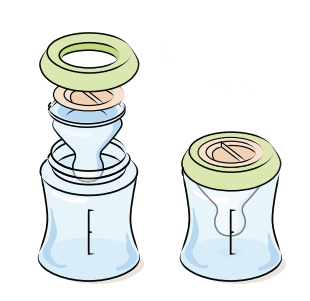
- If the items are not used right away, let them dry, and store them in a clean place. They could be kept on a clean and dry towel on the counter with another clean towel over them. They could be stored in a new plastic bag. Do not touch the inside of equipment where formula will have contact. Fit nipples, caps, and rings together. Put the nipple on the inside of the bottle to keep it clean until you are ready to use it.
It is safe to use home sterilizers that you can buy in the store. This includes microwave sterilizers. Be sure to follow the manufacturer’s instructions to make sure the plastics and metals will be safe. A pot on the stove also works well. Dishwashers do not normally sterilize formula equipment.
If you are using a disposable bottle system, wash all the non-disposable parts like nipples and caps and then sterilize them. New liners are clean and ready to use for one-time use only.
Automatic formula preparation machines for use at home are NOT recommended. The water that is used may sit dormant for a long time. More bacteria may grow in this water. When the water is heated, it is not hot enough to kill bacteria that may be in powdered formula. These machines also do not consistently mix powdered formula well.
Choosing Water to Make Formula

For concentrated liquid and powdered formulas, it is safe to use these waters after you sterilize them (see page 9):
- Tap water from your village, town or city.
- Bottled water that you can buy.
- Well water that has been tested regularly. This water must have safe bacteria levels and have proper nitrate levels. Be sure the nitrate concentration of well water is below 45 mg/L (or 10 mg/L measured as nitrate-nitrogen). If the water is high in nitrates, boiling it will increase the amount of nitrates even more. High levels of nitrates are very dangerous for babies under six months of age. Call or email your local health unit about using well water to prepare formula, or, if you have questions about your water supply.
If there is a boil water advisory in your community, buy water and sterilize it (see page 9). Some areas have problems with blue-green algae. If your area is experiencing high algae levels, use bottled water that you sterilized to mix formula. Boiled tap water will NOT be safe. Be ready for an emergency like a long power outage. Be ready by having enough ready-to-feed formula for 72 hours.
Please note:
- Home water treatment equipment does not replace the need to sterilize water for babies.
- Use the cold water tap. To be safe, first run the cold water for two minutes to flush away toxins. Hot tap water may contain metal toxins, such as lead from the pipes. For safe preparation, water needs to be boiled. If the water is high in lead, boiling it will increase the concentration of lead even more. To learn more about lead pipes, or a filter for houses with lead pipes, look here: www.hc-sc.gc.ca/ewh-semt/pubs/water-eau/lead-plomb-eng.php.
Do NOT use these waters for formula:
- Softened water which is high in sodium.
- Mineral water which is high in sodium and other minerals.
- Carbonated water: Carbonation and added flavours are not appropriate for babies. Carbonated water may also have added salt.
- Waters in areas that have naturally high levels of fluoride (higher than the guideline of 1.5 mg/L).
The safety of the following types of water for formula is not known so do NOT use:
- Purified water.
- Distilled water.
- Water treated by reverse osmosis.
- Deionized water.
- Demineralized water.
- Specialty nursery or baby waters.
Note: If you do not have a safe water source, use ready-to-feed liquid formula.
How to Sterilize Water, Choose Formula and Bottle-Feeding Supplies
Sterilize all water used for formula for babies of any age.
There is no research that says when to safely stop sterilizing. That means it is safest to sterilize water and bottle feeding supplies as long as your baby is using formula.
To prepare water for formula:
- Bring water to a rolling boil in a pot, on the stove. Continue to boil for two minutes. Do not use kettles that shut off before the water has boiled for two minutes.
- If you are using liquid concentrate formula:
- Boil water for two minutes and cool it before mixing it with formula.
- Water may also be sterilized by boiling for two minutes and then stored. Sterilized water may be kept in a sterilized, tightly closed container for 24 hours at room temperature or for 2 – 3 days in the fridge. Feed your baby formula that is close to body temperature.
- If you are using powdered formula:
- Bring your water to a rolling boil for two minutes. Then mix it with formula when the water is at least 70°C (1 litre of water cools to about 70°C after about 30 minutes, but it is different for different types of pots and amounts of water). When water is less than 70°C it is not hot enough to kill harmful bacteria in the formula. Cool the mixed formula quickly to body temperature before feeding your baby.
- For babies not “at risk” as written on pages 5 and 12, you can mix powdered formula with water that was sterilized, cooled, and stored in a sterilized, tightly closed container as above. This must be fed to your baby right away.
Selecting formula cans:
- Make sure that the formula container is not dented or bulging because these are signs that the formula may have gone bad.
- Check the expiry date on the can. Do not use formula after the expiry date.
Selecting bottle-feeding supplies:
- Watch your baby and use a nipple that helps your baby feed in a stress-free, relaxed way. For more on feeding cues and stress cues see page 18.
- Bottle nipples can be different shapes and sizes.
- The flow rate of a nipple is how fast the milk or formula comes out. The flow rate plus the size of the nipple hole may be different from one nipple to another, even for nipples in the same package.
- Different nipples work better at different times. Buy one package and watch that your baby is relaxed while feeding. If your baby is having problems, try a different type.
- Bottle nipples can be made of various materials.
- Check bottle nipples often. Replace them when they are cracked, sticky, torn, discoloured or if the hole gets larger and the formula drips out quickly.
For babies not “at risk” (see top of page 12), you can mix powdered formula with water that was sterilized and cooled. This must be fed to your baby right away.
Preparing Ready-to-feed Liquid Formula
Ready-to-feed liquid formula is the safest formula especially for premature infants, low birth weight infants, babies who are ill, or babies whose immune system may be weak. This type of formula is sterile.
- Wash your hands with soap and warm water, and sanitize the counter area according to the directions on page 6.
- Have all your sterile supplies ready (see pages 6 and 7).
- Wash the top of the can with hot water and soap, using a clean dishcloth.
Shake the can or bottle well and open with a sterilized can opener if needed.

Pour the formula directly into clean and sterilized bottles. Do not add water.
Use sterilized tongs to pick up nipples, caps and rings and put these on the bottles
Tighten the ring with your hands. Be careful not to touch the nipple.
Read guidelines on how and when to feed your baby later in this booklet.
Preparing Concentrated Liquid Formula
Concentrated liquid formula is sterile. Concentrated liquid formula mixed with water according to directions, is the next safest type of formula to feed your baby.
- Wash your hands with soap and warm water, and sanitize the counter area according to the directions on page 6.
- Have all your sterile supplies ready (see pages 6 and 7).

1. Wash the top of the can with hot water and soap, using a clean dishcloth.
2. Shake the can well and open with a sterilized can opener if needed.
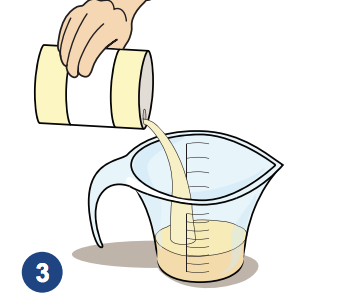
3. Measure the formula in a sterilized measuring cup. Read the label to see you how much formula and water to use.
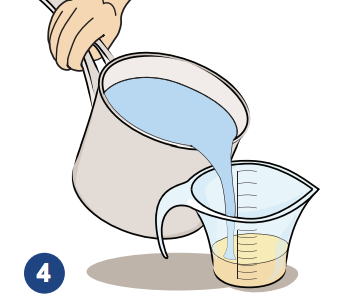
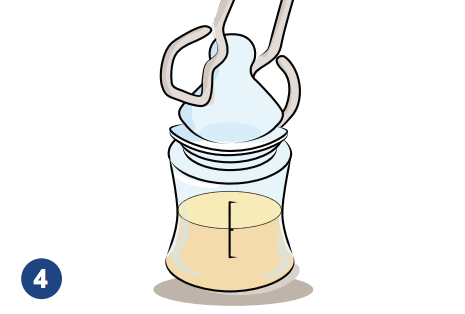
4. Add sterilized water which has been cooled down to room temperature.
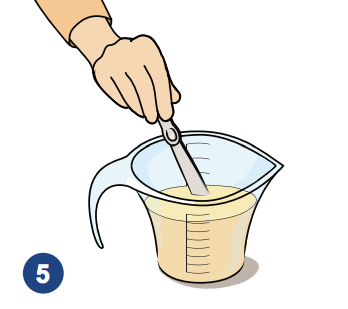
5 .Mix gently with a sterilized utensil.

6. Pour the formula into sterilized bottles.
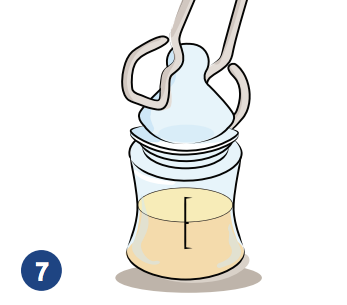
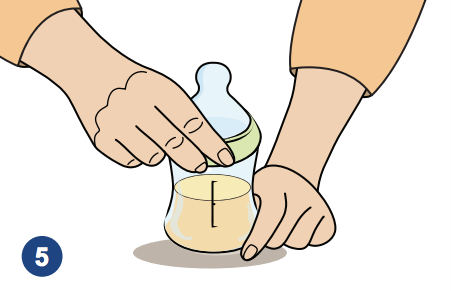
7. Use sterilized tongs to pick up nipples, rings and bottle caps.
8. Tighten the ring with your hands. Be careful not to touch the nipple.
Read guidelines on how and when to feed your baby later in this booklet.
Preparing Powdered Formula
Powdered formula is not sterile and has made some babies sick. It is important to prepare powdered formula correctly to lower the risk of your baby getting sick. The cost of liquid concentrate, bought by the case, and the cost of powdered formula are very similar once mixed (see page 3).
Babies who have the greatest chance of infections should have sterile liquid formula such as ready-to-feed or liquid concentrate formulas.
Babies at greatest risk of infections from powdered infant formula are those who:
- Are premature.
- Had low birth weight and are under two months of age.
- Have a weakened immune system.
If you are not sure about feeding your baby powdered formula, check with your health care provider. If you absolutely have to feed powdered formula to a baby with one or more of these risks, follow the directions very closely.
Directions:
- Wash your hands with soap and warm water, and sanitize the counter area according to the directions on page 6.
- Have all your sterile supplies ready (see pages 6 and 7).
Use sterilized hot water to make powdered formula. It is best to make the formula fresh and use it right away after it has cooled.
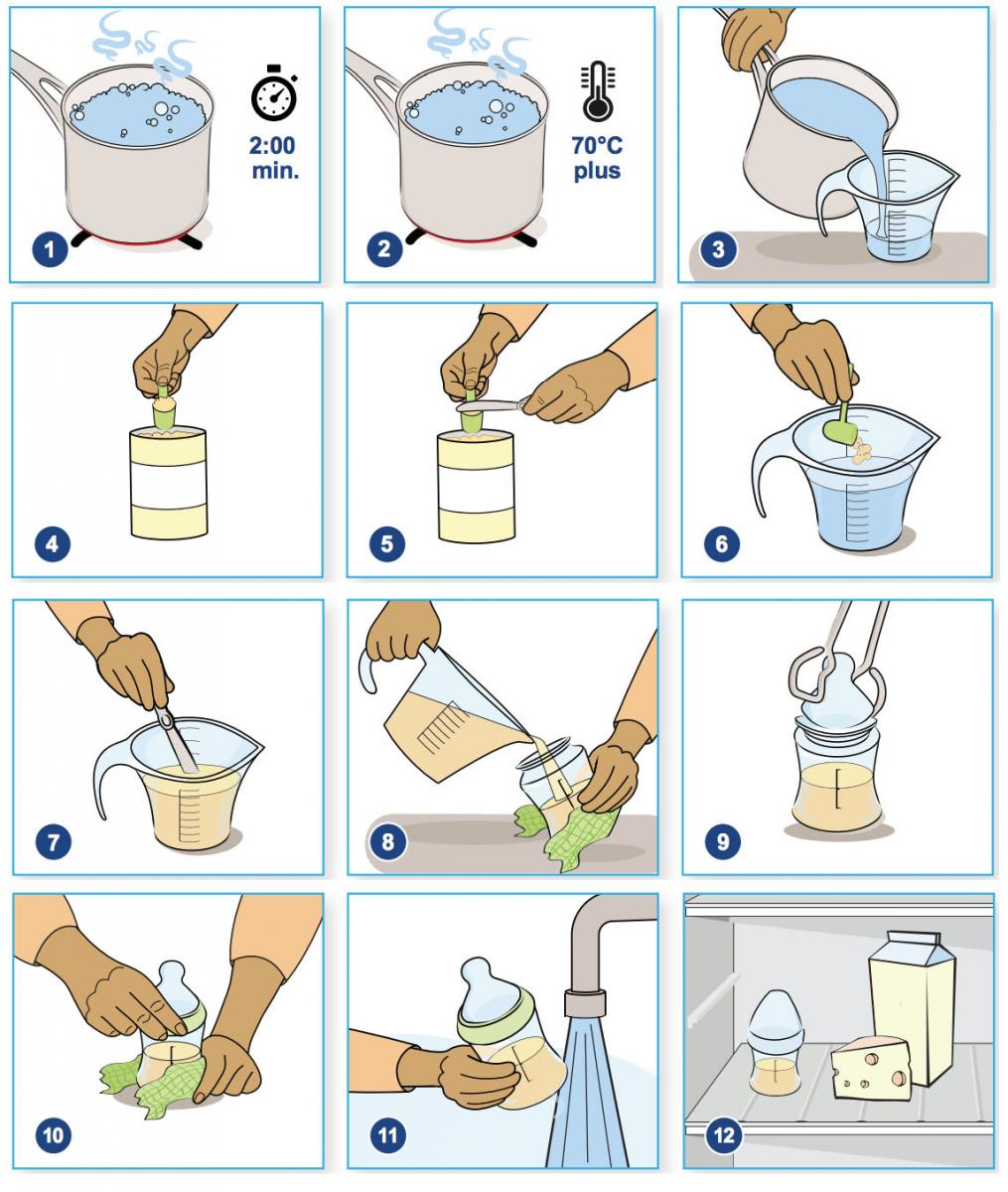
1. Boil the water for two minutes.
2. Make the formula when the water temperature is at least 70°C. The temperature must be over 70°C to kill harmful bacteria that may be in the powder. If the boiled water has been sitting at room temperature for more than 30 minutes, you will need to reheat it to 70°C or more before mixing it with formula.
3. Read the formula label. It will tell you how much formula and water to use. Pour the needed amount of sterilized water into a sterilized glass measuring cup.
4. Measure the needed amount of powdered formula. Use the scoop from inside the can
5. Do not pack the powder down into the scoop. Level the scoop with the flat side of a sterilized knife.
6. Add powder to the sterilized hot water.
7. Mix with a sterilized utensil until no lumps of powder are left.
8. Pour the amount of formula for one feeding into a sterilized bottle.
9. Use sterilized tongs to pick up nipples, rings and caps, and put on bottles.
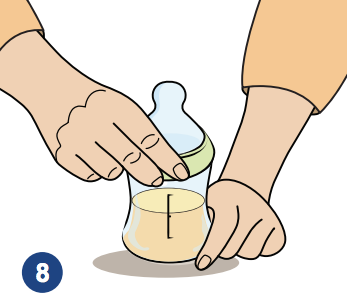
10. Tighten the ring with your hands. Be careful not to touch the nipple.
11. Quickly cool the bottle of formula under cold, running water or in a container of cold water. When it is at body or room temperature, feed your baby.
12. It is better to mix this type of formula fresh for each feed. If for some reason this is not possible, put the prepared formula in the fridge. Use it within 24 hours. Read guidelines on how and when to feed your baby later in this booklet.
Safely Storing Formula
- It is best to use formula immediately after preparing it.
- If formula has to be stored, begin with putting a label on the can. On the label put the date and time when the can was opened.
Ready-to-feed and Concentrated Liquid:
- Stored in Containers:
- Cover cans with a plastic cap or plastic wrap.
- Keep opened cans of concentrated and ready-to-use formula in the fridge.
- Throw cans out after 48 hours or as your label tells you on the can.
- Stored in Bottles:
- Keep bottles with formula in the fridge for 24 hours at the most.
- Throw out prepared formula after 24 hours.
- Store bottles near the back of the fridge where it stays cooler.
- Powdered Formula:
- Keep bottles with formula in the fridge for 24 hours at the most.
- Store open cans of powder with the lid tightly closed, in a cool, dry place (not in the fridge).
- After a can is open, use the rest of the powdered formula within one month, and before the expiry date.
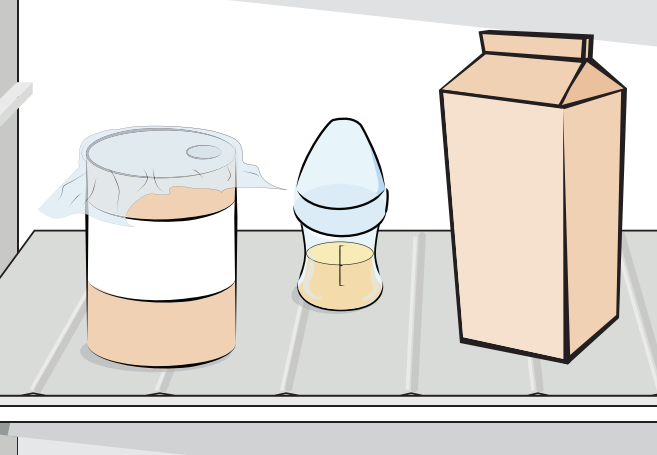
Never freeze formula to use later as this can change the texture and nutrition levels.
Warming Formula to Feed
Warming
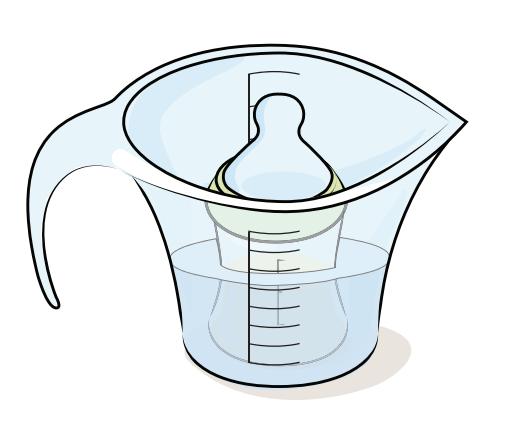
- Remove the formula from the fridge just before you need to feed your baby.
- Many babies prefer formula at body temperature (warm), and others like it cool. Either way is fine. Your baby will let you know what he prefers.
- Warm the bottle of formula in a container of warm water, or a bottle warmer. Keep the nipple area out of the water.
- Do not heat any bottles in the microwave.
- This heats the formula and creates “hot spots” that could burn your baby’s mouth.
- Warm the bottle for no more than 15 minutes. Shake the bottle a few times during warming.

- Check to make sure the formula is not too hot before the feeding. Put a few drops of formula on the inside of your wrist. It should feel slightly warm, not hot.
- Once you have warmed the formula, feed your baby right away.
- Do not reheat formula during a feed or refrigerate a partly used bottle.
- A bottle should be used within two hours of heating, or as it tells you on the can.
- Throw out any leftover formula.
When to Feed Your Baby
In the first few months of life, most babies eat at least eight times in 24 hours. This does not mean they feed every three hours. They will feed when they are hungry. They will feed during the night, and it is normal to feed during the night for many months. Older babies may need to eat less often. It is important to follow and respect what your baby is telling you. These are your baby’s cues. Follow your baby’s behavior.
Have your baby in your room with you whether in hospital or at home. It is recommended that your baby sleeps in your room on her own sleep surface for six months. This is best because it can:
- Help you notice when your baby is hungry.
- Help you better learn your new role as a parent.
- Help lower the risk of Sudden Infant Death Syndrome, also known as SIDS.
Your baby will tell you when he is hungry. It is important to understand these cues. It is best to feed when your baby is showing early feeding cues.
Feed your baby when you see early signs of hunger such as:
- Stirring, moving arms.
- Rapid eye movements under the eyelids.
- Mouth opening, yawning, lip smacking.
- Turning her head towards you or something that is touching her cheek, with her mouth open (rooting).

This is a good time to feed your baby.
Your baby is much hungrier when you see:
- Hands going to her mouth.
- Sucking or licking movements.
- Restlessness.
- Soft cooing or sighing sounds, getting louder.

Moderate Feeding Cues: Restlessness, sighing sounds getting louder
Late feeding cues showing your baby is extremely hungry include:
- Fussing.
- Crying.
- Being agitated.
- Exhaustion.
- Falling asleep.

Late Feeding Cues: Fussing, crying, agitated.
If your baby is showing late feeding cues, you may have to calm her down or let her sleep briefly before feeding. One great way to calm your baby is holding her skin-to-skin against your chest.
How to Bottle Feed Your Baby

- Cuddle or hold your baby close when feeding. Make feeding a special time.
- Hold your baby in an upright position, so that her head is much higher than her body, keeping the head supported.
- Put the bottle nipple just below the lower lip and wait for an “invitation” to put the bottle in. The invitation is your baby responding to this touch with a big, wide-open mouth. Ensure much of the nipple is in the baby’s mouth so that during feeding, your baby has a wide open mouth on a large part of the nipple. Avoid just pushing the nipple of the bottle into your baby’s mouth.
- Tilt the bottle only a little, keeping it almost flat, so that it is easier for your baby to manage the flow of the formula. Some air in the nipple will not cause a problem for your baby.
- Do not prop a bottle or put your baby to bed with a bottle. Your baby may drink too much or too little and it can also cause choking, tooth decay (cavities), and ear infections. It is important for babies to be held and touched during feeding.
- Hold your baby in one arm for some feeds and in another arm for others. This helps your baby with muscle development while he is turning his head to look at you.
- Feeding is a special time. Enjoy your baby, talk to her, smile, sing, cuddle.

Skin-to-Skin
Hold your newborn baby skin-to-skin every day. Continue to hold your baby skin-to-skin often during the first few months.
Research shows that spending lots of time skin-to-skin can:
- Help your baby feel safe and secure.
- Keep your baby warm.
- Stabilize your baby’s heart rate, breathing and blood sugar after she is born.
- Keep your baby calm and decrease crying.
- Help you to recognize when your baby is hungry.
- Help mothers, family members and babies learn to respond better to each other.
- Help babies learn to socialize better.
- Help brain development.
- Decrease postpartum depression for mothers.
Partners and other caregivers in the family can also enjoy skin-to-skin time with their babies. Practice during feeding time, bath time, when your baby is fussy, or any time. See: http://library.stfx.ca/abigelow/skin_to_skin/skin_to_skin.parents.mp4.
Feed According to Your Baby’s Cues
Pace the feeding so that it is at a rate comfortable for your baby. Your baby should look relaxed while feeding. Watch for a calm face and relaxed hands and arms, especially after the feeding starts. Do not rush the feeding. Take your time and do not force your baby to feed more than he wants. It is important to watch your baby’s cues. Watch for signs of discomfort or stress during feeding.
Signs of stress during feeding may be:

- Milk leaking or dribbling out of his mouth.
- Choking or gagging while feeding.
- Gulping or swallowing quickly without taking a breath after each swallow.
- Breathing fast or working hard to catch a breath.
- Smacking or squeaking noises.
- Squirming or struggling during the feed.
- Pushing the bottle away with his hands or tongue or moving his head away.
- Stressed look on his forehead.
If your baby shows signs of stress during a feed, slow down the feed for a few moments or stop. Give your baby a break by tilting the bottle so that less milk is in the nipple, or maybe no milk is there for a short while. You can also take the bottle out of his mouth, cuddle your baby, burp your baby, and watch for signs of hunger to restart. Restart the feed when your baby’s breathing is relaxed and your baby is asking for more. Watch for feeding cues (page 16). If there are feeding cues, continue feeding. If there are no more feeding cues, end the feeding. If your baby keeps showing signs of stress during feedings, check if your feeding supplies are right for your baby. For example, the flow of milk from the nipple you are using may be too fast. If you have trouble fixing the problem, get help from a knowledgeable professional.
Stop the feeding when your baby shows signs of fullness.
These include:
- Slowing down or stopping sucking.
- Closing his mouth.
- Turning his head away.
- Pushing away from the bottle or the person feeding him.
- Falling asleep and no longer interested in feeding.
Do not pressure your baby to finish a bottle. Pay attention to your baby’s feeding cues and let your baby decide how much or how little to eat. Be responsive to your baby. Your baby may still have small sucking movements after a feed. This is normal baby behaviour.
Burping
- Try to burp your baby just for a few minutes part way through the feed and after the feed.
- Burping may bring up air that was swallowed during a feed.
Signs that your baby needs to burp are:
- Arching his back.
- Getting cranky or fussy.
- Pulling away from the bottle.
- Sucking slows down or stops.

Burp your baby by gently patting his back with a cupped hand. Try these positions to burp your baby:
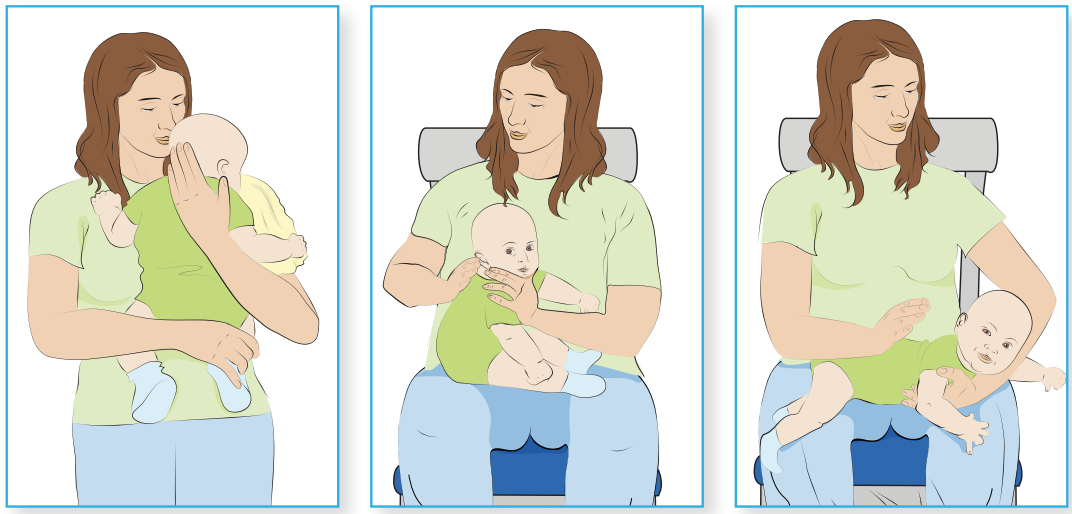
- Hold your baby upright over your shoulder.
- Hold your baby in a sitting position on your lap. Your baby will be leaning slightly forward with your hand supporting his jaw.
- Place your baby on his stomach across your lap
After the feeding:
- Throw out unused formula. Never reuse, reheat or put it in the fridge to use later. Leftover formula may start to grow harmful bacteria after two hours.
- Rinse the bottle and bottle parts right after the feeding.
- Clean your baby’s gums with a clean, warm, damp cloth after each feeding.
- As your baby grows, wipe his gums and brush his teeth to help prevent cavities. Be sure to start bringing him to the dentist from when he is one year old.
Feeding Your Growing Baby
Feeding in the first week:
- In the first few days your baby’s stomach is quite small. Your baby will need only small amounts of formula at each feeding.
- Each baby is different in how much they want to feed and how often. Feed your baby whenever she shows signs of being hungry. See page 18 for more on baby’s feeding cues. With time you will better learn how to tell if your baby is hungry.
- Do not try to force your baby to finish a bottle or a certain amount. Like adults, babies are different in the amount they want at each feeding. It is better to feed small amounts and more often.
- As your baby grows during the first few weeks, she will take more at a feeding.
- Mothers may wonder if they are feeding their baby too little or too much. Respond to your baby’s feeding cues and if you have questions speak to your health care provider.
- If you have questions or concerns about feeding your baby, talk to your health care provider.
Feeding after the first week:
- Expect your baby to feed often in the first month or so. After that, your baby may go longer between feedings and then will drink more at each feeding.
- Feed according to your baby’s cues, not certain amounts.
- Growth spurts are common at about three weeks, six weeks, three months and six months. Your baby may want more formula at these times or may want to feed more often.
- Babies do not need a vitamin D supplement if they only receive formula, because formula has added vitamin D. Talk with your health care provider to find out if your baby needs added Vitamin D.
- Many health care providers use growth charts to track babies’ measurements. Try not to compare your baby to other babies. Babies grow at different rates. Growth charts for babies may be viewed at: www.dietitians.ca/secondary-pages/public/who-growth-charts.aspx. See “Is My Child Growing Well?”
Transporting Formula
- It is safest to travel with unopened ready-to-feed formula.
- The next safest is to prepare water for your formula at the place you are going. If you are unsure of the safety of the water where you are going, bring safe water from home that has been boiled. Make sure it is being stored and transported in a sterilized container.
- If you must prepare the formula ahead, only take a bottle with you after it is cooled to fridge temperature, which is about 4°C.
- Whenever possible, place the formula in a refrigerator once you reach where you are going.
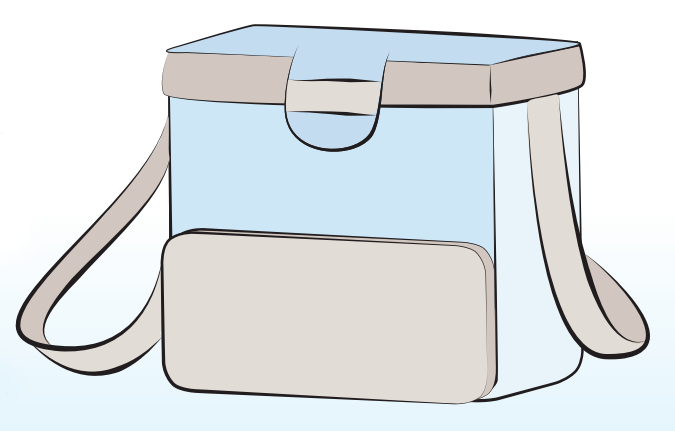
- If there is no refrigerator available, keep the formula in the cooler bag until feeding time.
- When formula has been out of the fridge, it is safest to use it within two hours.
- The bottle of formula can be put back in a fridge for up to 24 hours from the time it was prepared as long as you can answer “yes” to each of these statements:
- 1. The bottle of formula has been kept cold while travelling.
- 2. The bottle of formula has been out of the fridge for less than 2 hours.
- 3. The baby has not taken any formula from the bottle, even only a few mouthfuls.
Acknowledgements

The booklet was adapted with permission from Niagara Region Public Health. We would also like to thank Hamilton Health Sciences for their contribution. Thanks go as well to members of the BFI Strategy Implementation Committee, and the many professionals who provided input. Thank you to Marg La Salle, BFI Assessor for her contributions. Finally, a big thank you goes to mothers who reviewed this document.
Booklet contact information:
To order copies, or for copyright or reproduction information, contact the BFI Strategy at bfistrategy@tehn.ca.

This document has been prepared with funds provided by the Government of Ontario. The information in this document reflects the views of the authors and is not officially endorsed by the Government of Ontario. The Best Start Resource Centre, Michael Garron Hospital and the Provincial Council for Maternal Child Health do not necessarily endorse the resources and services listed in this resource. The advice provided in this resource does not replace health advice from your health care provider. This document was completed in 2017.